What Did the FDA Say?
The FDA 3rd Party Service Report
G. Wayne Moore, B.Sc., MBA, FASE
6/12/18
Co·her·ence, noun – the quality of being logical and consistent.
For those anticipating the above in the report released by the FDA my sincere condolences. For those believing that the report was affirmation on their particular point of view on the subject – well, don’t take the victory lap quite yet. As a regulatory professional let me try and unpack a few of the key elements of the report and specifically a few of the potential implications of the Agency’s carefully crafted words. The key words found in the Executive Summary section of the FDA report that define which way the FDA intends to proceed on a go-forward basis are:
• Promote
• Clarify
• Strengthen
• Foster
Conspicuously absent from the list of verbs above is the long-anticipated active verb; “Regulate”. In spite of that glaring omission I did find refreshing their admission that regulatory requirements are, in their words, “burdensome”. Indeed, regulatory requirements are burdensome by design, and by definition; as they are intended to ensure, as much as reasonably possible, that medical devices are both safe and efficacious for their intended use to both benefit patients and to protect patients and users from harm. These requirements extend to OEMs from design and development – through servicing the finished device once it is introduced into interstate commerce. The FDA concluded in its report that both OEMs and 3rd Party service entities equally provide “…high-quality, safe, and effective servicing of medical devices”, and because of that they will not “impose” the same “burdensome” service regulations on 3rd Party servicers that they currently impose on OEMs. Consistency would dictate that if two parties are providing equal service, and “…there is insufficient objective evidence to conclude there is a widespread public health concern related to servicing…” that either, (a) the regulations apply to both, or (b) the regulations apply to neither.
On Page 19 of the report, the FDA estimates there are between 16,520 and 20,830 firms in the United States performing medical device servicing. The FDA does not need to “estimate” how many firms in the United States are medical device OEMs because – they know the exact number, they know who they are, where they are, and what they make. Because of the registration and regulatory blind-spot currently present with 3rd Party servicers all the FDA can do is guess how many there are, where they are, and what they are actually doing – this “guessing” approach is inconsistent with regard to ensuring patient safety.
So, with the FDA concluding there will be no regulation/registration of 3rd Party servicers why do I say 3rd Party servicers should not be taking a victory lap quite yet? Look no further than Page 4 of the report where the FDA states; “…FDA believes it has the statutory authority to regulate device servicing.” This means that although the Agency currently does not exercise that authority; “…FDA has generally not enforced FD&C requirements with respect to servicing activities…”, and implying in the report that this policy will continue in the future relative to 3rd Party servicers, they could decide at any point, without any notification, to start exercising that authority. If they do exercise that authority and decide to inspect a 3rd Party’s facility – what will the criteria of the inspection consist of? What specifics will the 3rd Party be held liable for in its operation and QMS? Without having those specifics, the 3rd Party would not know in advance if it is in or out of regulatory compliance. This non-determinism is the proverbial sword of Damocles over the head of every 3rd Party servicer in the US. Please note above that the FDA used the term “generally”, generally not enforced does not mean never enforced. 3rd Parties need to seek immediate clarification from the FDA on what would trigger an inspection (for any reason other than “for-cause”) and what parts of the QSR 3rd Party servicers would be held accountable to during an inspection. FDA outlines on Page 24 the course it intends to pursue relative to an informal rather than a formal regulatory servicing QMS structure (see paragraph just before Section 6.2).
The Agency gave perhaps a small hint of what they were thinking concerning at least peripherally regulating 3rd Party service by their announced intent to pursue a more comprehensive clarification between servicing and remanufacturing in the form of a Guidance Document (see Page 24). My sense is that there are numerous 3rd Party servicers who really believe they are simply repairing or servicing medical devices when, in actuality, they are performing work that meets the current FDA definition of remanufacturing for a given device. Unlike 3rd Party servicers, companies performing remanufacturing, as defined by the Agency, must register as such, and must follow the 510(k)-submission process as a remanufactured device is considered a new device which must have a cleared 510(k) for that device prior to being re-introduced into interstate commerce. If the device isn’t cleared then it is considered by the FDA as an adulterated device, subject to both recall and sanctions against the offending company. My suggestion to all 3rd Party servicers is to take a very close and objective look at what work you are currently performing and what parts and materials you are using to effect repair and match those up with the definition of a remanufactured device. You can do that by downloading the 510(k) clearance Guidance documents from the FDA website for the particular medical device you are repairing. In either the broader text of the Guidance, or in an Appendix of the Guidance you will generally find what they consider the parameters of remanufacturing.
One of my take-aways from the FDA docket and subsequent report is that all 3rd Party servicers should, at a minimum, be certified to ISO13485-2016 for the work they are performing relative to medical devices. Additionally, it is my view that supply-chain managers and HTM professionals in hospitals should also, at a minimum, demand their suppliers be ISO 13485-2016 certified. Sadly, I find far too many hospitals saying they choose vendors based on; (1) Quality, (2) Cost, and (3) Availability, when in actual practice it is; (1) Cost, (2) Availability, and (3) Quality.
Throughout the course of this docket several 3rd Party servicers stated over-and-over that they were currently performing excellent work and in the same breath they were demanding OEMs (see Page 19 last sentence prior to Section 5) provide them with training, parts, manuals of every description, system software diagnostics, and other “information” all at what they describe as “fair and reasonable” prices – although fair and reasonable is at best subjective – for example they want to only pay for what it costs to make another copy of a service manual without even considering the extensive time and effort put into developing the manual in the first place! The OEMs were, in my view, unfairly vilified throughout this docket as greedy and anti-competitive – trying to put 3rd Parties out of business, which is of course nonsense as OEMs often augment their field service by utilizing qualified 3rd Party servicers – a point that even the 3rd Parties brought up. In short, this entire Docket shifted from being a search for an optimal regulatory or QMS solution for after-market medical device repair, to a zero-sum game between stakeholders that drove the wedge between OEM, HTMs, and 3rd Party servicers even deeper, rather than bring them together. If that animus continues then it would appear highly unlikely that any actions by the FDA to “foster evidence development” between the stakeholders will go anywhere, or produce anything meaningful.
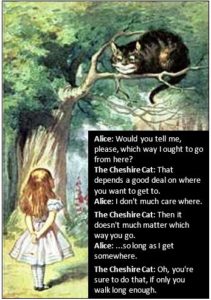
Twenty years ago, the FDA punted on the question of servicing and now twenty years later they have, in my estimation, done so once again – albeit with more flowery sounding language. From these two data points one can conclude that perhaps in the year 2038 the FDA will look at this issue again – maybe then they will get it right – or Alice’s words will once again ring true. So, no one should be taking a victory lap on this FDA report as it really doesn’t address the core issue of patient safety, rather we should all reflect on what our core mission is in this market – delivering and maintaining safe and effective medical devices for patients, and what we are doing to improve our part in the process. Anyway, check back with me in 2038 for an update.
Until next month,
Wayne
About the Author, G. Wayne Moore:
A 30-year veteran of the diagnostic ultrasound market Wayne has held senior level positions with several major medical equipment manufacturers, including Honeywell Medical Systems and Siemens Medical Solutions. Wayne has been directly involved in the development and commercialization of more than 15 technologically intensive ultrasound systems. He is widely published in diagnostic ultrasound literature, a sought after speaker at medical imaging conferences, has served as an expert witness in multiple ultrasound litigations, and holds more than 16 United States ultrasound related patents. Wayne obtained his MBA from the University of Denver – Daniels College of Business.
He was elected as a Fellow of the American Society of Echocardiography (FASE) in 2009.
Acertara Labs
Correspondence: Dave Dallaire
1900 South Sunset Street, Suite F, Longmont, CO 80501, USA
Email: [email protected]
www.acertaralabs.com
